A common practice millions of Americans partake in to stay healthy is actually doing much more harm than good and may be contributing to the spread of drug-resistant disease.
Infectious Disease Research
Stephen Trent and his colleagues have developed 61 new strains of genetically engineered bacteria, which may improve the efficacy of vaccines for diseases such as flu, pertussis, cholera and HPV. “For a long time vaccinology was really a trial-and-error field. We knew certain things worked. But we didn’t entirely know why. Now that’s changing.”
Accelerating the evaluation and development of new vaccines for emerging health threats is the goal of George Georgiou, Edward Marcotte, Andrew Ellington and Gregory Ippolito, who are working on a $6.5 million contract from the U.S. Department of Defense and the Defense Threat Reduction Agency. “The contract is significant because it will help us develop a new paradigm for vaccine evaluation,” says Georgiou.
Robert Krug and his team discovered that a protein produced by the influenza A virus helps it outwit one of our body’s natural defense mechanisms. That makes the protein a potentially good target for antiviral drugs directed against the influenza A virus. Better antiviral drugs could help the millions of people annually infected by flu, which kills up to 500,000 people each year.
Sara Sawyer co-authored a study that explains a novel way to engineer key cells of the immune system so they remain resistant to infection from HIV. The new approach could ultimately replace drug treatment, in which patients have to take multiple medications daily to keep the virus in check. “Instead of the cocktail of multiple drugs, we provide these cells with multiple antiviral genes,” Sawyer says.
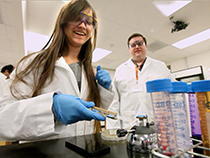
Jason Shear and his colleagues developed a novel 3-D printing technology to build protein “cages” around bacteria in gelatin. The structures allow researchers to study how communities of bacteria, such as those found in the human gut and lungs, interact and develop infections. “What the technology allows us to do is put [bacteria] in conversation with each other, in very precise ways, and see what happens.”
Chris Sullivan is working to outwit the evolutionary strategies of viruses, like herpes and HIV, that form persistent lifelong infections but are often seemingly dormant in our bodies. His research focuses on understanding how latent viruses hide from our adaptive immune response, and whether there are any vulnerabilities that might be exploited to make them visible, so that we can kill them all.
The solution: Don’t buy a product simply because it says it’s “antimicrobial.”
Products made using triclosan — a common antibiotic found in everything from hand soap to cleaning wipes to toys — are among microbiologist Marvin Whiteley‘s biggest pet peeves.
“The problem with that antibiotic is that it’s really not that active against a lot of the bugs you’d hope it would be,” says Whiteley, a professor of molecular biosciences. But it’s not triclosan’s ineffectiveness that bugs Whiteley. It’s that it weakens other antibiotics.
“Bacteria that are susceptible to triclosan become resistant to it, but they also become resistant to antibiotics you might get at the doctor’s office. So you’re proliferating antibiotic resistance,” he warns. “We’re putting millions of pounds of this stuff into the environment.”
Understanding what makes bacteria resistant is just one facet of the work being done on infectious disease at UT. Whiteley and the students in his lab study complex and opportunistic infections that have more than one

“In the mid-1900s we were worried about ‘professional pathogens’ that just made people sick” with conditions like measles or whooping cough — diseases now preventable thanks to vaccines. “Vaccines are one of the biggest feats that increased life expectancy,” Whiteley says.
(Related: Read about College of Pharmacy’s Maria Croyle‘s groundbreaking work on a vaccine for ebola.)
But as certain infections become nastily persistent — and often, resistant to available treatments — physicians have fewer options. That’s where Whiteley’s research comes in. His lab looks at how bacteria previously thought to not be important in disease can make an infection worse or harder to treat.
“Other bacteria present in an infection can influence how pathogenic the infection is,” Whiteley says. Doctors may not be looking at the whole stew of bacteria when they make a diagnosis and “may assume the other bacteria are innocuous, but they’re not. We try to understand how the secondary bacteria are influencing the primary infection.”

This work includes bacteria in the mouth (“Periodontitis is one of the most prevalent bacterial diseases in the world,” Whiteley says), chronic wounds (“Seven to 10 percent of the U.S. health care budget is spent on treating wounds,” he says, such as bedsores or diabetic injuries), and burn wounds, which have a high mortality rate.
Understanding infectious disease is nearly as complex as the infections themselves.
“The questions we’re talking about are rooted in ecology, evolution, things way outside of my own discipline,” Whiteley says. “You might need an evolutionary biologist, an ecologist, a physicist, a chemist, a biologist and always engineers who are thinking more practically about problems.”
That need for a team of experts working together was one of the driving forces behind the creation of UT’s new Center for Infectious Disease, a research unit that spans three colleges (Natural Sciences, Engineering and Pharmacy). Whiteley is the founding director.
“One of the great things about UT is that it’s big,” says Whiteley. “That’s also a problem. The center will get people together with an interest in infectious disease, regardless of department. You can’t have 30 people working independently of one another; you have to have a common goal.”
Support the research of
the Center for Infectious Disease
The Center is supported in part by the John Ring LaMontagne Memorial Chair in Infectious Disease and Global Health.
The center is poised to take advantage of the establishment of Dell Medical School, which will give researchers the opportunity to see their lab work tested in clinical settings.
“There’s not one thing UT infectious disease researchers could have asked for better than having a medical school,” Whiteley says, “because that was the thing we lacked: that direct translational, clinical application of what we do.”
Other researchers in the center include Stephen Trent, George Georgiou, Robert Krug, Sara Sawyer, Jason Shear and Christopher Sullivan. (See the sidebar on the right for more information about their work.)
In the meantime, Whiteley advises, stay away from triclosan. “I’m not sure wiping the handle on your HEB cart is going to save your life.”
You may also like:
You Are Your Microbiome (The Texas Scientist)
Lauren Meyers: Crunching the Numbers to Stop a Pandemic (Longhorn Game Changer)
More stories about infectious disease research (College of Natural Sciences)
This story is part of a yearlong series “In Pursuit of Health,” covering medical news and research happening across the university.
This article is by Cory Leahy and originally appeared here: http://www.utexas.edu/know/2014/05/05/back-with-a-vengeance-the-trouble-with-defeating-diseases/



















Comments