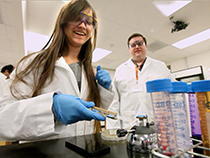
The problem with chronic wounds, and the solution, may lie in the war between two bacteria, says Marvin Whitely.
 By studying the war between two bacteria, microbiologist Marvin Whiteley has found part of the answer to one of the most expensive mysteries of modern health care: Why don’t chronic wounds heal? That’s no small thing when it comes to a problem that immiserates the lives of more than six millions American every year.
By studying the war between two bacteria, microbiologist Marvin Whiteley has found part of the answer to one of the most expensive mysteries of modern health care: Why don’t chronic wounds heal? That’s no small thing when it comes to a problem that immiserates the lives of more than six millions American every year.
“It’s estimated that as many as one in 50 Americans will suffer from a chronic wound during their lifetime,” says Whiteley, associate professor of biology in the College of Natural Sciences. “We don’t fully understand why these wounds won’t heal, but a compromised immune system is clearly relevant. Diabetes and obesity are major risk factors, as is getting older.”
Whiteley comes at the problem of these wounds, defined as those that don’t heal in predictable stages over a period of three months, from two angles.
The microbiologist has been studying the pathogenic bacterium Pseudomonas aeruginosa, for most of his career. It is one of the most common bacteria in the world, is present in most chronic wounds, and is notoriously resistant to antibiotics.
“Pseudomonas is everywhere,” he says. “We’ve all been exposed to it. Many of us have had small infections, from a cut or from a burn. One way you can tell if you’re infected by Pseudomonas is if you notice a bluish color to your wound. It makes a bluish pigment. But if you have a healthy immune system you probably cleared it just fine.”
The other angle for Whiteley is historical. In particular the 19th century work of his hero, the French chemist and microbiologist Louis Pasteur.
“One hundred and fifty years ago Pasteur wrote a whole paper about how we really need to be thinking about complex infections and what microbes are there,” says Whiteley. “He actually cured anthrax infections by inoculating animals with Pseudomonas. But once genetics came around everyone started focusing on single bugs, and we forgot about what Pasteur had said. Now I think we need to go back and try to understand what a real infection looks like, and I think most real infections harbor more than one kind of bacterium."
In most chronic wounds the two primary “bad guys” are Pseudomonas and Staphylococcus aureus. When both are present, wounds tend to be more resistant to antibiotics than if just one of them were there. Whiteley has just figure out why.
“What we’ve figured out is that Pseudomonas can detect Staph, and when it does it increases its virulence,” he says.
By genetically manipulating and then testing different Pseudomonas mutants, Whiteley discovered that the bacteria detect what are essentially the waste products of growth in Staph as well as other similar bacteria.
“Staph has a really thick cell wall that protects it,” he says. “It’s kind of like a really thick chain link fence. As it grows it has to break that fence to divide, and as that happens some pieces float away. Pseudomonas has evolved to detect those pieces of broken fence, and it knows that if it sees them then there is a gram positive bacterium around it, invading its space. It responds by becoming very aggressive.
This increased virulence leads to increased resistance to the body’s natural immune response.
“This isn’t the only mechanism responsible for chronic wounds, but I believe it’s a significant one,” says Whiteley, “and it points in the direction of ways that treatments might be improved.”
Whiteley says that one possibility is that it may make more sense to treat a wound that is infected by both Pseudomonas and Staph by giving antibiotics targeted only to Staph. The idea would be that as the Staph diminishes or disappears, the Pseudomonas would become less virulent. Then our immune system would have a much better chance of clearing it on its own.
Currently, he and his lab members are investigating the plausibility of this and other new approaches to treating chronic wounds. They’re also planning to expand their study of chronic wounds beyond just the activity of the two main actors, Pseudomonas and Staph, to include other potential supporting players.
“Pasteur was on the right track, but he didn’t have the technology to pursue it in the way we do now,” says Whiteley. “That’s what I’d like to do now, understand real infections in their real complexity.”















Comments