
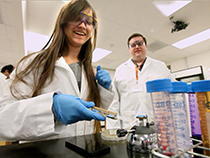
When microbiologist Marvin Whiteley and graduate student Matthew Ramsey began peering into the human mouth, as part of an ongoing quest to understand more about the ways that bacteria form complex ecologies, they didn’t know what they would find. They just knew that they liked what the mouth had to offer.
“One of the nice things about your mouth is that it’s colonized by bacteria on day one,” says Ramsey, a fourth-year student in Whiteley’s lab. “A lot of these bacteria are found only in a human or primate host, and they always have to live around each other. It’s a really rich environment in which to look at multi-species interaction.”
What Whiteley and his lab have ended up discovering, over the past few years, has more than vindicated their hopes for the mouth. Most recently, in a paper published in the Proceedings of the National Academy of Sciences, Whiteley and Ramsey reported their discovery of one particular oral bacteria that takes its cue from another oral bacteria about when to start defensive action against our immune system.
This was the first time, says Ramsey, that scientists have ever seen one bacteria initiating an immunoprotective action in response to a signal from another bacteria.
“Usually,” he says, “bacteria will look for cues in their environment and respond accordingly. They’ll look for the presence of specific types of sugars and carbohydrates that indicate the onset of a host immuno-response. We haven’t previously seen immunoprotective factors up-regulated by a cue from a separate species of bacteria.”
The particular bacteria they were interested in, in this case, is Aggregatibacter actinomycetemcomitans. It lives in the mouths of about half of Americans, and is harmless as long as one maintains a decent level of oral hygiene (or doesn’t suffer from certain medical conditions, like diabetes).
If conditions in the mouth get bad enough, however, Aggregatibacter can end up playing a significant role in periodontitis, which is a nasty form of gum disease that’s common in the developing world.
With this over-arching concern in mind, Whiteley and Ramsey set out to learn what happened when Aggregatibacter was cultured in the presence of Streptococcus gordonii, one of a number of strains of common bacteria that also inhabit the mouth.
What they found were two changes in Aggregatibacter when it was grown alongside S. gordonii. One was that Aggregatibacter produced catalase, an enzyme that decomposes the hydrogen peroxide that S. gordonii produces. This was anticipated, says Ramsey, because without the ability to break down hydrogen peroxide, Aggregatibacter wouldn’t be able to live for long.
“The other thing we saw,” says Ramsey “was that the gene apiA was up-regulated in Aggregatibacter. That was the big deal.”
It was a big deal, says Ramsey, because apiA acts to bind a protein known as factor H, which is the same protein that many human cells use to signal to the immune system that they should be left alone.
“It mimics what human cells do,” says Ramsey. “It’s how your own cells keep your immune system from attacking them.”
That apiA can bind factor H has been known since 2003. What hasn’t been documented, before Ramsey and Whiteley’s recent paper, was that apiA could take its cue to bind factor H from another bacteria.
This is significant, says Ramsey, for a number of reasons. The better we can understand the mechanism whereby Aggregatibacter protects itself from our immune response, the better equipped we’ll be to fight it.
More generally, the better we understand how bacteria communicate with each other, the more likely we are to be able to disrupt or modify that communication.
“Even if it’s one particular bacterium that’s causing an infection, it’s not happening in isolation,” says Ramsey. “Understanding these complex polymicrobial relationships is essential to formulating strategies for preventing infection.”
At a more basic science level, the discovery is a step forward in understanding how bacteria evolve in the context of complex microbial communities.
“These bacteria have probably been evolving together for a long time,” says Ramsey, “and although it’s still a hypothesis, we suspect that it’s easier for bacteria to evolve to talk to each other than to look for information in a host environment.”
News
From the College of Natural Sciences
Oral Fixations
Graduate student Matthew Ramsey is working with Dr. Marvin Whiteley to better understand the complex ecologies of bacteria living in the human mouth.















Comments