A diagnostic tool called the MasSpec Pen has been tested for the first time in pancreatic cancer patients during surgery. The device is shown to accurately identify tissues and surgical margins directly in patients and differentiate healthy and cancerous tissue from banked pancreas samples.
At about 15 seconds per analysis, the method is more than 100 times as fast as the current gold standard diagnostic, Frozen Section Analysis. The ability to accurately identify margins between healthy and cancerous tissue in pancreatic cancer surgeries can give patients the greatest chance of survival.
The results, by a team from The University of Texas at Austin and Baylor College of Medicine, are published this week in the Proceedings of the National Academy of Sciences.
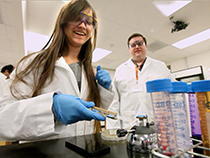
"These results show the technology works in the clinic for surgical guidance," said Livia Schiavinato Eberlin, an assistant professor of chemistry at UT Austin who leads the team that invented the pen, in collaboration with James Suliburk, head of endocrine surgery at Baylor. "Surgeons can easily integrate the MasSpec Pen into their workflow, and the initial data really supports the diagnostic accuracy we were expecting to achieve."
The most common type of pancreatic cancer, pancreatic ductal adenocarcinoma, spreads rapidly and is highly lethal, with a five-year survival rate of 9% for all stages. The most effective treatment option is surgical removal of the tumor.
Cancer surgeons face a dilemma: It's often difficult to tell good tissue from bad. If any cancerous tissue is left behind, there's a risk the tumor will regrow, potentially requiring the patient to undergo additional rounds of surgery, radiation or chemotherapy, and decreasing the chances of survival. On the other hand, removing too much healthy tissue, especially from vital organs, can also compromise a patient's health. Determining the margin between healthy and cancerous tissue is critical to a successful surgery.
For this study, the investigators first used the MasSpec Pen to analyze 157 banked human pancreatic tissues to develop and evaluate the technology in the laboratory for pancreatic cancer. Then, the investigators moved the system to the operating room at Baylor St. Luke's Medical Center in Houston, which is affiliated with Baylor College of Medicine, where the surgeons tested the technology in 18 pancreatic surgeries. The pen has been tested in more than 150 human surgeries to date, including for breast and thyroid, and results of those additional tests will be submitted for publication soon.
Mary King, a graduate student and the study's first author, and other members of the Eberlin research group operated the mass spectrometer during surgery.
A typical surgery to remove a pancreatic tumor can take from 6 to 12 hours.
"Surgery of the pancreas is a very complex and detailed surgery that requires numerous intraoperative decisions over several hours that can have long-lasting effects on oncologic outcomes for patients with pancreas cancer," said George Van Buren, M.D., associate professor of surgery at Baylor and one of the surgeons who performed operations during the experiment. "The MasSpec Pen technology opens the door for real-time, precision medicine to be performed in the operating room at a level that has never been seen before."
These are the first published results of intraoperative use of the MasSpec Pen, in other words, on intact or just-removed tissue from patients during surgery. Preclinical research published about the technology in 2017 led to widespread enthusiasm and interest, including from writers in Hollywood who adapted the idea for a segment on the television program "Grey's Anatomy."
The researchers plan eventually to submit the design to the U.S. Food and Drug Administration for approval as a medical device.
Banked tissue samples were provided by the Cooperative Human Tissue Network and Baylor.
This work was supported in part by the National Cancer Institute of the National Institutes of Health, and by the Gordon and Betty Moore Foundation. Livia Eberlin receives support for research in her lab from the Cancer Prevention and Research Institute of Texas.
King, Suliburk, Eberlin, Jialing Zhang and others are inventors in US Patent No. 10,643,832 and/or in other patent applications related to the MasSpec Pen technology licensed by The University of Texas to MS Pen Technologies Inc. and its subsidiary Genio Technologies. Zhang, Suliburk and Eberlin are shareholders in MS Pen Technologies Inc.
The University of Texas at Austin is committed to transparency and disclosure of all potential conflicts of interest. The university investigator who led this research, Livia Schiavinato Eberlin, has submitted required financial disclosure forms with the university. Eberlin is a co-founder with an equity stake in MSP Technologies, an inventor-led startup formed to commercialize the MasSpec Pen technology, owned by the university.
NOTES TO REPORTERS:
1) When the study publishes, it will be available at: https://doi.org/10.1073/pnas.2104411118
2) Images and videos associated with this news release are here: https://utexas.box.com/s/977b13ex0stdsovi7cgud6z5561a2556
3) Press contacts: Marc Airhart, University of Texas at Austin, 512-232-1066, mairhart@austin.utexas.edu and Dipali Pathak, Baylor College of Medicine, 713-798-6826, Dipali.Pathak@bcm.edu
Further Background:
Each type of cancer cell produces different levels of small molecules called metabolites and other biomarkers that act as fingerprints, setting it apart from healthy cells. Once the surgeon touches the MasSpec pen to the tissue, the device measures these fingerprints in a few seconds with a tool called a mass spectrometer that the pen is connected to. In this study, the investigators used the software that they trained with the database of molecular fingerprints gathered from the human tissue samples analyzed in the lab, both cancerous and healthy, to evaluate the data acquired in surgery.
Mary King noted that for the physicians, integrating the tool into surgery was easy and non-disruptive to their workflow.
"Training the clinicians how to use the device simply involved showing them how to properly hold the pen to tissue during an analysis," King said. "It's been very simple for them to learn and start collecting mass spectrometry data themselves during surgery.'"
"Being in the clinic has allowed us to recognize what are the critical issues for surgeons, more than being in the lab," Eberlin said. "As scientists, we may think certain things are important, but surgeons see it from a different perspective with a focus on improving clinical workflow and outcome for patients."
The study's other authors from UT Austin are: Jialing Zhang, John Q. Lin, Kyana Y. Garza, Rachel J. DeHoog, Clara L. Feider, Alena Bensussan, Marta Sans, Anna Krieger, Sunil Badal, Michael F. Keating and Spencer Woody. Other authors from BCM are: Sadhna Dhingra, Wendong Yu, Christopher Pirko, Kirtan Brahmbhatt and William E. Fisher.

















Comments