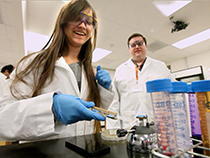
The National Institutes of Health (NIH) has awarded a team led by Richard M. Crooks, a chemistry professor at The University of Texas at Austin, a $2 million grant to develop an inexpensive, at-home test for people diagnosed with heart failure.
Heart failure is a chronic disease in which the weakened heart can't pump enough blood to meet the body's need for oxygen. More than 5 million people in the U.S. suffer from heart failure, with symptoms that can include difficulty breathing, sudden weight gain, dizziness and confusion.
Crooks is developing an affordable, do-it-yourself test that can inform heart-failure patients how stressed their hearts are within minutes. When the heart is stressed, it releases certain chemical biomarkers. The current procedure for diagnosing and monitoring the severity of heart failure includes measurement of a biomarker at a pathology lab where patients have blood drawn and then consult with their cardiologist to obtain the results after the blood is analyzed. Many people who suffer from heart failure are poor, elderly and/or live in rural areas without good transit to pathology labs. For them, it can be difficult to undergo this process.
Crooks and his team have already tested a pre-prototype of the heart-failure sensor, with encouraging results.
When perfected, the sensor Crooks develops will provide feedback to patients about the progression of their disease. It will also warn a patient that dire symptoms, which might trigger a costly emergency room visit, might be imminent.
"It's very similar to the way that diabetics monitor their glucose levels at home to ensure that they are managing their disease effectively," Crooks said. "Except instead of doing it three or four times a day, it would probably be used just once each week."
A heart-failure patient would prick his or her finger and place a drop of blood on the end of a disposable paper test strip and insert it into an electronic device. The blood would interact with a substance imprinted on the paper that creates an electrochemical signal in the presence of the heart-stress biomarker.
"And then a couple of minutes later, a light would come on that's like a traffic signal," Crooks said. "If it's green, you're good. If it's yellow, you probably ought to make an appointment with your cardiologist. And if it's red, you should head directly to the emergency department of the hospital."
Crooks noted that people diagnosed with heart failure are often told to change their diets. But changing habits can be hard.
"Something that our device could provide is very quick feedback to them saying, yes, whatever you're doing is the right thing or whatever you're doing, it's the wrong thing," he said. "That kind of quick feedback is known to be very effective for changing habits."
Crooks said this device fits in with a bigger trend in health care.
"All of health care is going towards home health care," he said. "In 10 years, all the things you go to the doctor for now — colds, flus, you name it — you'll be doing some preliminary diagnosis at home. It puts more responsibility on you, but that can be empowering."
The project received its first round of funding in 2015 when UT Austin's Dell Medical School awarded Crooks and his team a Texas Health Catalyst award. In addition to seed funding, the program introduced them to potential funders and provided a consultant to help ensure that their design could meet guidelines for approval by the Food and Drug Administration.
The latest NIH grant will allow Crooks and his team to build a prototype of the device. Within two years they plan to start testing blood from human subjects suffering from heart failure. The results will be compared with those from the conventional biomarker test performed by a clinical pathology lab, the current gold standard.
















Comments