The brain's primary immune cells play a fundamental role in alcohol use disorder, according to a new study from Scripps Research and The University of Texas at Austin. The scientists are the first to link these cells—known as microglia—to the molecular, cellular and behavioral changes that promote the increased drinking that's associated with alcohol dependence.
More than 14 million adults in the United States are considered problem drinkers, characterized by an impaired ability to stop or control their alcohol use despite unfavorable social, occupational or health consequences. The new study, which appears in the journal Biological Psychiatry, points to a potential new approach for treating the widespread condition. The paper is "in press," meaning it has been peer reviewed and accepted, but is awaiting final formatting.
"There were hints that glial cells are important in alcohol dependence but it was not clear if the changes in neuroimmune cells like microglia are secondary to prolonged alcohol abuse rather than causal," said Adron Harris, professor of neuroscience at UT Austin and director of the Integrative Neuroscience Initiative on Alcoholism (INIA)-Neuroimmune consortium. "This study suggests a causal role for microglia."
"Not only are microglia partly responsible for the drive to consume alcohol, but they regulate the neurons responsible for these behavioral changes," said co-first author Sophia Khom, a neuroscientist in the Scripps Research laboratory of senior author Marisa Roberto. "If you remove these cells, you can prevent dangerous alcohol consumption and the resulting damage to the brain. In essence, you can hit the reset button."
Friend or foe?
Microglia are prevalent throughout the brain, performing useful functions required for our health. Once seen simply as "brain glue" that didn't serve much purpose, they are now known as dynamic cells that reduce inflammation and alleviate other disease symptoms as they clear away cellular debris from brain tissue.
However, dysfunctional microglia are implicated in a number of devastating brain disorders such as Alzheimer's, Parkinson's and Huntington's. They have been thought to play some role in alcohol use disorder, but scientists weren't sure of the extent to which they're implicated in disease onset and progression.
In experiments involving mice that were conditioned to become alcohol-dependent, the scientists administered an investigational drug known as PLX5622, currently in clinical trials, that removes microglia from the brain. This stopped the mice from increasing their alcohol intake and lowered anxiety-like behavior associated with alcohol dependence. Among its other effects, the drug also dampened signals from genes that regulate production of a brain chemical called GABA (short for gamma-aminobutyric acid) that's known to be critical in the development of alcohol dependence.
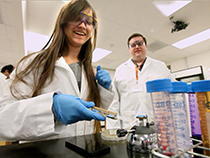
"It has finally become clear that microglia are, in fact, important for escalations in drinking, changes in neuronal function and detrimental changes in the brain's immune response to alcohol," said co-first author Anna S. Warden, a neuroscience graduate student in the labs of R. Adron Harris and R. Dayne Mayfield at UT Austin and the Waggoner Center for Alcohol and Addiction Research.
Scripps Research and University of Texas at Austin began their collaboration as part of the INIA consortium, funded by National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism. Harris is the overall director of the consortium and Roberto is a scientific director of the consortium.
"Most people know someone struggling with alcohol use disorder. Yet, very few effective treatments exist, and our team is resolved to change that," said Roberto. "With this study, we are one step closer to developing a treatment to help individuals with alcohol use disorder. We are incredibly hopeful that this discovery can be translated into an effective therapy."
Inching closer to a treatment
With their promising findings in hand, the scientists plan to continue melding classical neuroscience techniques with neuroimmunology—a newer field combining neuroscience with the study of the immune system—to advance their novel approach to treating alcohol use disorder.
More specifically, Roberto said, the goal would be continuing the investigation to develop immune-targeting therapies and understanding how different cell types are regulating neurons' response to alcohol.
"What factors are telling a neuron to change its function?" Roberto asks. "If we can target this communication, then we can prevent neurons from undergoing the changes that result in alcohol use disorder."
Authors of the study, "Microglia control escalation of drinking in alcohol dependent mice: Genomic and synaptic drivers," are Anna S. Warden, Sarah A. Wolfe, Sophia Khom, Florence P. Varodayan, Reesha R. Patel, Michael Q. Steinman, Michal Bajo, Sarah Montgomery, Roman Vlkolinsky, Tali Nadav, Ilham Polis, Amanda J. Roberts, Roy D. Mayfield, Robert A. Harris and Marisa Roberto.
This work was supported by the National Institutes of Health/National Institute of Alcohol Abuse and Alcoholism. The drug PLX5622 was provided by Plexxikon Inc.
This post is based on a press release by Scripps Research.

















Comments