We asked you, dear listeners, to send us your most burning questions about COVID-19. And you didn't disappoint. You asked: When will it be safe for my 12-week-old baby to meet her grandparents? Can you catch it twice? Is the virus mutating and will that make it harder to develop vaccines? In today's episode, our three experts get to the bottom of these questions, and more.
Meet our experts:
Professor Lauren Ancel Meyers is an epidemiologist and leader of the UT COVID-19 Modeling Consortium. Her team recently found that the virus was circulating in China and in Seattle, Washington weeks earlier than previously thought.
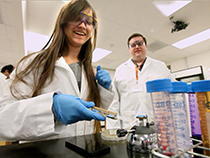
Greg Ippolito is a research assistant professor of molecular biosciences and an expert on how our immune systems respond to pathogens. He is working with doctors at Houston Methodist Hospital to test the efficacy of a potential COVID-19 treatment called convalescent plasma therapy.
Jason McLellan is an associate professor of molecular biosciences whose team created a critical component in several COVID-19 vaccines currently in clinical trials. He and his team is also developing a therapy for COVID-19 based on special antibodies from llamas.
Music for today's show was produced by:
Podington Bear - https://www.podingtonbear.com/
TRANSCRIPT
MA: This is Point of Discovery. I'm Marc Airhart. COVID-19 continues to spread here in Texas, and around the world. Here at The University of Texas at Austin, we have scientists working hard on modelling the spread of the virus -- advising decision makers on ways to flatten the curve -- developing vaccines and other treatments -- and more. We want to share their expertise with you. So a few weeks back we asked you to send us your most burning COVID-19 questions.
MA: First up, I reached out to Professor Lauren Ancel Meyers, an epidemiologist and leader of the UT COVID-19 Modeling consortium to help with this question. Ashley asks: "Let's say most people in a crowd are wearing masks, but a few aren't. How safe is the group?"
LM: The more people that wear face masks, the safer the group is. If one person is infected and one person is susceptible, it's more important that the infected person wears a face mask because it sort of blocks the virus from leaving their mouth and going out into the air near where other people are. So you know the reason we're encouraging everyone to wear face masks is because infected people often don't know they're infected, right? Because they could be perfectly asymptomatic or maybe they just have mild symptoms. For every person who doesn't wear a face mask, you know, it's one extra chance that you could have an infected person that can be spreading disease to the others in the crowd.
MA: Annette writes: "We have a 12-week-old baby. When will it be safe for her to meet her grandparents?"
LM Yeah, it's a hard question. I mean, one of the most important things we can do right now is protect people who are particularly vulnerable to this virus. So these are people who are over age 65, or are younger but have a known underlying condition that puts them at higher risk for severe outcomes, higher risk of ending up in the hospital or worse. And so, you know, I think if you have family members that fall into any one of those categories, It's best to err on the side of caution. If you do want to visit with me to try to do it in a safe way outdoors at some distance. Or if you want to have more kind of intimate interactions, ensure that you've really kind of quarantined yourself to the best [of] your ability for the last couple of weeks before you go out and have those close interactions. My recommendation is just try to be as safe as possible, but certainly find ways to safely be with the people who you want to spend time with.
MA: I asked Professor Meyers one question of my own: Why is COVID so hard to contain?
LM: So there's two things that make this pandemic so difficult to contain. And those two things are the speed with which this virus spreads, and the fact that it often spreads silently, or we don't even know somebody is infected and spreading to others. So this thing, in comparison to SARS 1, the original SARS virus that was spreading in the early 2000s, that virus never caused a pandemic -- it caused a series of small epidemics around the world. But why were we able to contain those outbreaks in a way that we're not able to contain COVID-19? Well, first of all, SARS 1 took about twice as long to spread. The typical person, if they were infected, they went on to infect somebody else. There's typically about eight days between that first infection and the second infection. With COVID-19, it's much shorter, it's probably about four or five days between somebody becoming infected then infecting somebody else. So it's happening at a much faster pace, which means you really have to race to try to contain outbreaks when they happen. And then the other thing that we were just talking about is that it often spreads silently. With SARS one, people were not infectious until they were clearly very ill, until they themselves knew they were sick. So there wasn't this early period of time where they could be walking around silently spreading to others, we knew they were sick, we could contain them. We could identify all their cases, we had time to track their contacts, we had time to track them down and isolate them. With COVID-19, by the time someone has developed symptoms, they may have already spread the disease to several other people. … it's why we have to assume that we and the people around us might have been exposed and could potentially be infectious if we really want to stop this virus. It's why we need to wear face masks, even when we feel perfectly healthy.
MA: Rosalinda Lam asks: "Can you get it twice?"
GI: Personally, I am not an adherent to the idea that we can get COVID-19 a second time.
Ma: That's Greg Ippolito, a research assistant professor of molecular biosciences and an expert on how our immune systems respond to pathogens.
GI: I think that some of what we have seen in the press is, in fact, stemmed from tests that can have false positive results. Or even if they're genuine positives, these tests measure the presence of virus, RNA, the virus's nucleic acids, but not live and infectious virus itself. The test is more just, it's almost detecting corpses of the virus that might still be harbored in the nasopharynx of infected individuals [but weeks after their infection with the virus].
MA: He noted that humans have encountered other coronaviruses before. Studies of people infected with one of those, SARS (or "SARS classic"), offer clues about how long immunity might last after infection with the current coronavirus.
GI: there have been long-term follow-up studies since 2002-03, studies over the years of SARS classic survivors, and indicates that there is a spectrum of sustained immunity for years following the initial and likely only infection, where I think even 75% of those SARS classic survivors still had antibodies circulating in their blood three years after the infection. And then there were still survivors who had antibody circulating out even to six years post infection. Mind you, by six years, a majority of the survivors had lost the majority or even all of their antibody. Still, that's one to six years of potential protection by antibody, if past is prologue.
MA: So people infected with the novel coronavirus might have antibodies for one to six years after. That could buy them critical time until there's a vaccine. There's a third reason to be optimistic, Ippolito said. A study published in the journal Science earlier this month suggests that another kind of immune cell -- called memory T-cells -- might help some people who were previously exposed to other coronaviruses that cause the common cold to fight off this novel coronavirus too. Finally, he pointed to a fourth reason for hope. Just look at other respiratory viruses like the flu. He noted that they infect us over and over and over again.
GI: We know that there the human immunity is not lifelong. And people are re-infected with these viruses repeatedly … throughout life. Nonetheless, we also know that if we have pre-existing immunity, or we've been infected once with that respiratory virus, that typically the next time we see it, and the next time we see it, that the severity of disease diminishes with the repeat infections. And if that is the case with COVID-19, that is reason to be cheerfully optimistic and hopeful.
MA: Next I called up Jason McLellan, associate professor of molecular biosciences, whose team created a critical component in several COVID-19 vaccines currently in clinical trials. Listener Carol Rowley wanted to know whether SARS-CoV-2 is mutating, and if so, does that affect how dangerous it is or make it harder to develop vaccines?
JM: The coronavirus does mutate like a lot of RNA viruses. So over time, they start to accumulate mutations in their genetic backbone. This can lead to changes in the various proteins that they produce. And so, this is occurring, but so far, we haven't really seen any effect on the transmissibility of the virus or its capacity to cause more severe illness. So it'saccumulating some changes, not at a frequency that is alarming, or that would suggest a vaccine made against an earlier strain would no longer work against some of these newer variations.
MA: Another listener pointed out that vaccines normally take years to develop and yet we already have dozens of candidates developed in just a few months. How were they created so fast?
JM: So it's in part because people have been working on coronavirus vaccines for decades or so after the SARS coronavirus outbreak in 2002, there was a lot of effort investigating coronaviruses, trying to understand how to make vaccines and we've learned a lot. And then after the MERS coronavirus outbreak in 2012, there was renewed interest, new technologies had become available. And so conceptually, it's actually pretty straightforward to make a coronavirus vaccine, we know that the spike protein is the major target of the human antibody response. So we need to present the spike protein, or a fragment of the spike protein to the human immune system. And it's just a matter of choosing how best to do that.
MA: So it helped that you and others had already spent years studying coronaviruses?
JM: Exactly. Yeah, some of the vaccines people have already tested out a lot of the platforms for MERS coronavirus. And some of the some of the work we've done with MERS purified proteins. Our colleagues at the NIH were working with Moderna on mRNA-based MERS coronavirus vaccines, so it's really just swapping out the MERS spike for the SARS CoV-2 spike. So, conceptually it wasn't very difficult. It's just how fast can you do it? And all the prior work has allowed us to get a head start on that. But that's really where this idea of basic science funding, trying to work on understanding all viruses and different things, so that way you have this background of knowledge for when an outbreak occurs. We have this knowledge we can draw on to immediately start making interventions. An outbreak is not the time to start years or decades worth of like primary basic science research.
MA: Thank you so much, Jason, and thank you for all your work you're doing for all of us.
JM: You're welcome. Thanks, Marc, for having me.
MA: Point of Discovery is a production of The University of Texas at Austin's College of Natural Sciences. Music for today's show is by Podington Bear. Special thanks to all the listeners who sent in questions and to our experts -- Lauren Ancel Meyers, Greg Ippolito and Jason McLellan. To read a transcript of this show and find links to COVID-19 research by today's guests, visit us on our website at pointofdiscovery.org. If you like what you heard, be sure and tell your friends. We're available wherever you get your podcasts, including Apple Podcasts, Google Podcasts, Stitcher and Spotify. Our senior producer is Christine Sinatra. I'm your host and producer Marc Airhart. Stay tuned and stay safe y'all!
About Point of Discovery
Point of Discovery is a production of the University of Texas at Austin's College of Natural Sciences. You can listen via Apple Podcasts, Spotify, RSS, Stitcher or Google Podcasts. Questions or comments about this episode or our series in general? Email Marc Airhart.














Comments