A widely used class of chemotherapy drugs, called topoisomerase inhibitors, come with some serious downsides: bone marrow damage, reduced blood cell production, diarrhea and heart damage. And some cancers can quickly develop resistance. A new discovery about a second class of drugs might lead to combination therapies that are just as effective, but with fewer downsides.
Researchers at The University of Texas at Austin studied naturally-occurring Bromodomain proteins, which are targeted by a class of anti-cancer drugs currently in Phase 2 human clinical trials, called BET inhibitors. It was already known from studies in cultured cancer tissue that BET inhibitors slow the proliferation of cancer cells by interfering with a process called transcription. But the researchers were surprised to find that these drugs also work in a second way that's similar to the way topoisomerase inhibitors work, by damaging the DNA of cancer cells so badly that they cannot repair it and then subsequently die.
"Based on this discovery, we think combining topoisomerase inhibitors and BET inhibitors might provide an opportunity for combination-based treatments that may still effectively target processes that cause DNA damage to kill cancer cells while reducing overall side effects of chemotherapy by reducing the dose of each" said Kyle Miller, associate professor in the Department of Molecular Biosciences at UT Austin, member of the Livestrong Cancer Institutes at UT Austin's Dell Medical School, and corresponding author of a new study in the journal Genes & Development.
There was a lot of excitement in the cancer research community in 2010 when the first BET inhibitor, JQ1, was shown to kill cancer cells in cultures. Several pharmaceutical companies have since jumped in and developed their own versions of BET inhibitors. But the road from promising laboratory compound to FDA-approved drug is long.
It's still not clear how effective BET inhibitors will be in humans, or whether they also have side effects. There are currently five BET inhibitors in Phase 2 human clinical trials for the treatment of various cancers: ZEN0003694 (prostate cancer); INCB057643 (lung and colorectal cancers); CPI-0610 (leukemia and a blood marrow cancer called myelofibrosis); BMS-986158 (advanced tumors); and GSK525762 (blood cancers, including acute myeloid leukemia, non-Hodgkin's lymphoma and multiple myeloma).
For more details on these and earlier stage BET inhibitor trials, search on clinicaltrials.gov.
Topoisomerase inhibitors have been used for decades in the clinic and are routinely prescribed for a range of cancers including: acute leukemia, multiple myeloma, Non-Hodgkin lymphoma, and cancers of the lungs, breasts, prostate, bladder, brain, blood, bones, thyroid, ovaries, cervix, testes and gastrointestinal tract.
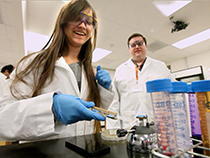
The study's co-first authors are Jae Jin Kim and Seo Yun Lee, postdoctoral researchers in the Miller lab in the Department of Molecular Biosciences at UT Austin. In addition to Miller, senior authors from UT Austin are professors Tanya Paull and Edward Marcotte, as well as associate professor Blerta Xhemalce, in the Department of Molecular Biosciences, and professor Jennifer Brodbelt, chair of the Department of Chemistry.
The latest study was carried out in cancer cells grown in culture. The researchers used molecular and cellular techniques to selectively deplete and study individual proteins belonging to a group called Bromodomain (BRD) proteins — some of which are targeted by BET inhibitors — to see what effects their absence had on cancer cells. They were surprised to find that 24 of the 42 human BRD proteins were involved in repairing damaged DNA, a function linked with cancer suppression.
"Our study points to a more wide-spread involvement and new functions for these proteins in protecting the integrity of our genetic information," Miller said.
Other authors of the study from UT Austin are: Fade Gong, Anna Battenhouse, Daniel Boutz, Aarti Bashyal, and Samantha Refvik. Cheng-Ming Chiang at the University of Texas Southwestern Medical Center is also a co-author.
Funding for this research was provided by the National Cancer Institute, National Institutes of Health, the American Cancer Society, National Science Foundation, Robert A. Welch Foundation and Army Research Laboratory. Funding was provided by the UT System in support of the UT System Proteomics Core Facility Network. Additional support was provided to Dr. Chiang by the Cancer Prevention & Research Institute of Texas (CPRIT).

















Comments