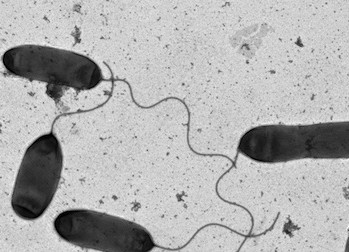
 Transmission electron micrograph of Vibrio cholerae. Image courtesy of Stephen Trent.AUSTIN, Texas — For 50 years scientists have been unsure how the bacteria that gives humans cholera manages to resist one of our basic innate immune responses. That mystery has now been solved, thanks to research from biologists at The University of Texas at Austin.
Transmission electron micrograph of Vibrio cholerae. Image courtesy of Stephen Trent.AUSTIN, Texas — For 50 years scientists have been unsure how the bacteria that gives humans cholera manages to resist one of our basic innate immune responses. That mystery has now been solved, thanks to research from biologists at The University of Texas at Austin.
The answers may help clear the way for a new class of antibiotics that don’t directly shut down pathogenic bacteria such as V. cholerae, but instead disable their defenses so that our own immune systems can do the killing.
Every year cholera afflicts millions of people and kills hundreds of thousands, predominantly in the developing world. The infection causes profuse diarrhea and vomiting. Death comes from severe dehydration.
“If you understand the mechanism, the bacterial target, you’re more likely to be able to design an effective antibiotic,” says Stephen Trent, associate professor of molecular genetics and microbiology and lead researcher on the study.
The bacterium’s defense, which was unmasked this month in the Proceedings of the National Academy of Sciences, involves attaching one or two small amino acids to the large molecules, known as endotoxins, that cover about 75 percent of the bacterium’s outer surface.
“It’s like it’s hardening its armor so that our defenses can’t get through,” says Trent.
Trent says these tiny amino acids simply change the electrical charge on that outer surface of the bacteria. It goes from negative to neutral.
That’s important because the molecules we rely on to fight off such bacteria, which are called cationic antimicrobial peptides (CAMPs), are positively charged. They can bind to the negatively charged surface of bacteria, and when they do so, they insert themselves into the bacterial membrane and form a pore. Water then flows through the pore into the bacterium and pops it open from the inside, killing the harmful bacteria.
It’s an effective defense, which is why these CAMPs are ubiquitous in nature (as well as one of the main ingredients in over-the-counter antibacterial ointments such as Neosporin).
However, when the positively charged CAMPs come up against the neutral V. cholerae bacteria, they can’t bind. They bounce away, and we’re left vulnerable.
V. cholerae can then invade our intestines and turn them into a kind of factory for producing more cholera, in the process rendering us incapable of holding onto fluids or extracting sufficient nutrients from what we eat and drink.
“It pretty much takes over your normal flora,” says Trent.
Trent says that scientists have known for some time that the strain of V. cholerae responsible for the current pandemic in Haiti and elsewhere is resistant to these CAMPs. It’s that resistance that is likely responsible, in part, for why the current strain displaced the strain that was responsible for previous pandemics.
“It’s orders of magnitude more resistant,” says Trent.
Now that Trent and his colleagues understand the mechanism behind this resistance, they hope to use that knowledge to help develop antibiotics that can disable the defense, perhaps by preventing the cholera bacteria from hardening their armor. If that happened, our CAMPs could do the rest of the work.
Trent says the benefits of such an antibiotic would be considerable. It might be effective against not just cholera but a range of dangerous bacteria that use similar defenses. And because it disarms but doesn’t kill the bacteria outright, as traditional antibiotics do, it might take longer for the bacteria to mutate and evolve resistance in response to it.
“If we can go directly at these amino acids that it uses to protect against us, and then allow our own innate immune system to kill the bug, there could be less selection pressure,” he says.
Trent’s lab is now screening for compounds that would do precisely that.
For more information, contact: Daniel Oppenheimer, College of Natural Sciences, 512 745 3353; Stephen Trent, professor, (512) 232-8371.















Comments